Lyme Disease
The Pennsylvania Department of Health and Centers for Disease Control and Prevention have additional information on ticks and Lyme disease, including a series of educational videos.
Other Names: Lyme borreliosis, erythema migrans
Cause
Lyme disease is a tick-borne disease of humans and some domestic mammals caused by the bacteria Borrelia burgdorferi. Wild mammals and birds are often asymptomatic reservoirs for the bacteria that rarely become ill. The first case of Lyme disease in the United States was described in 1969 in a Wisconsin grouse hunter. The disease got its name after an outbreak occurred in 1975 in children from Lyme, Connecticut, but the bacteria responsible for causing the disease was not identified until 1982.
Significance
Lyme disease can cause mild to severe illness in humans. It is common in Pennsylvania, particularly in areas where the Ixodes (black-legged ticks or deer ticks) are abundant. If left untreated, the illness can progress to serious conditions involving the joints, heart, and nervous system. Lyme disease is currently the most commonly reported vector-borne disease in humans in the United States.
Species Affected
B. burgdorferi has been isolated in many species of wild mammals and birds. In North America, the bacteria have been found in coyotes, raccoons, chipmunks, rabbits, and several species of rats, mice, and shrews. The bacteria have also been isolated in several bird species including but not limited to the mallard, ring-necked pheasant, wild turkey, house wren, song thrush, American robin, gray catbird, song sparrow, and house sparrow without causing disease. Domestic animals including dogs, cats, cattle, and horses can also become infected. The Lyme disease bacteria can cause a very similar illness in humans.
Distribution
Lyme disease is regularly reported in Japan, China, Western Europe, countries of the former Soviet Union, the United States, southern Canada, and Australia. Cases are occasionally reported in Africa and South America. Most cases occur in the northeast and mid-Atlantic region, but it has been reported in almost every state. In 2009, 95% of reported cases of Lyme disease in the US occurred in the following 12 states: Pennsylvania, New Jersey, New York, Massachusetts, Connecticut, Wisconsin, Maryland, Minnesota, New Hampshire, Delaware, Maine, and Virginia. The incidence of Lyme disease in domestic dogs in Pennsylvania currently varies between 10 and 13%, but no assays of deer mice have been conducted.
Transmission
The black-legged tick (Ixodes scapularis), also known as the deer tick, is the most important vector for B. burgdorferi in the eastern and Midwestern United States. The western black-legged tick (Ixodes pacificus) is the primary vector in the western US. Other tick species and biting insects such as mosquitoes, deer flies, and horse flies can also carry the bacteria, but it is still unclear how well they can transmit the bacteria to new hosts.
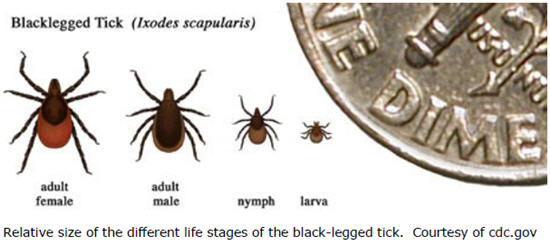
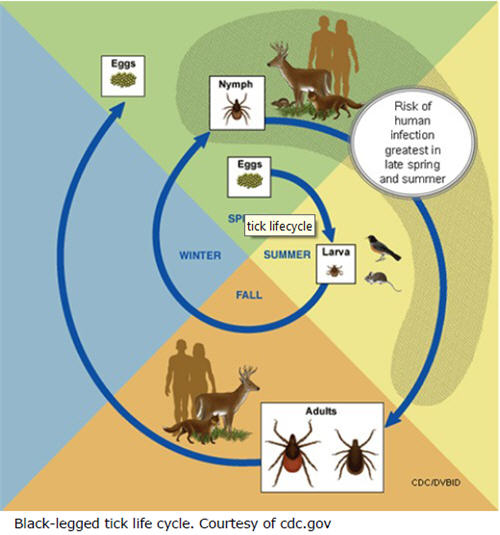
The tick life cycle plays an important role in the transmission of this disease. Black-legged ticks are known as "three-host" ticks because they feed on blood from three different vertebrate hosts at each of the three different stages in their lives. When the larvae hatch in the spring, they do not carry the B. burgdorferi bacteria. During the summer, the larvae feed on the blood of mice, squirrels, raccoons, rabbits, and other small vertebrates. The larvae mature into nymphs in the fall and hibernate over the winter. The larval and nymphal ticks can become carriers of the Lyme bacteria by feeding on wildlife reservoir hosts. White-footed mice (Peromyscus leucopus) and eastern chipmunks (Tamias striatus) are the most important reservoirs for B. burgdoferi in the eastern and Midwestern United States. If they acquired the bacteria as larvae, the nymphs can transmit the bacteria to new vertebrate hosts when they feed the following spring or summer. If not, they can acquire the bacteria as nymphs and infect other species in the fall of that year. The bacteria are typically transmitted to humans by nymphs. In the fall, the nymphs develop into adults that feed on their third and final host. Adults previously infected as larvae or nymphs can also transmit the bacteria to new hosts, including humans and domestic animals. Adult female black-legged ticks feed preferentially on deer to get energy to lay eggs, but deer do not act as reservoirs for the Lyme bacteria. Females lay eggs the following spring then both male and female adults die, and the cycle continues.
Clinical Signs
Most wild mammals and birds do not seem to show clinical signs of Lyme disease. The one exception to this is the white-footed mouse. White-footed mice may temporarily exhibit reddening of the ear and neurological signs including trembling, head tilt, circling to one side, loss of coordination, and weakness of the hind limbs. Some domestic animals, especially dogs, develop clinical signs including fever, stiffness, lameness, and arthritis. Less commonly, domestic animals may experience kidney, neurologic, eye, and cardiac problems. Humans with Lyme disease often (85% of the time) develop a "bull's eye lesion" (known as erythema migrans) at the location of tick attachment followed by fever, fatigue, and headache.
Diagnosis
Lyme disease is diagnosed using laboratory tests.
Treatment
Humans and domestic animals can be treated successfully with antibiotics, especially when the infection is addressed early. Wildlife species do not develop Lyme disease, so treatment is not considered.
Management/Prevention
People should take certain precautions to reduce the risk of contracting Lyme disease. When spending time outdoors in potential tick habitats, long pants tucked into socks or boots, and insect repellant are recommended. Each day spent in tick habitat should be followed by a thorough "tick check". Ticks found on people or pets should be removed promptly and completely. Veterinarian recommended tick control products should be used on pets that spend time outdoors. Lyme disease vaccines are no longer available for humans, but vaccines are available for pets.
Suggested Reading
Brown, R. N., and E. C. Burgess. 2001. Lyme Borreliosis. Pages 435-454 in E. S. Williams and I. K. Barker, editors. Infectious diseases of wild mammals. Iowa State University Press, Ames, Iowa, USA.
Centers for Disease Control and Prevention (CDC). 2011. Lyme Disease.
http://www.cdc.gov/lyme.
Michigan Department of Natural Resources. Wildlife Disease. Lyme Disease.
http://www.michigan.gov/dnr/1,1607,7-153-10370_12150_12220-26945--,00.html.
Lyme Disease & Deer - Revelation or Red Herring
- The black-legged tick (Ixodes scapularis) is the most important vector for Lyme disease transmission in the Eastern US. It has a 2-year life cycle consisting of 3 life stages: larval, nymph, and adult.
- Risk of exposure to Lyme disease is correlated with abundance of acorns, mice, and chipmunks – key hosts for subadult ticks and their corresponding food source.
- Deer are a dead-end host for the Lyme disease bacteria. They do not infect ticks with the bacteria that cause Lyme disease nor do they contract the disease when an infected tick feeds on them. They play no direct role in the transmission cycle.
- Adult ticks primarily feed on deer in mid-autumn to mate and acquire a final blood meal before females lay eggs to complete their life cycle.
- Larvae feed on mice, birds, and other small mammals in the summer and early fall. Nymphs also feed on mice, birds, and other small mammals but are most active in the late spring and early summer.
- Tick populations are not affected by deer abundance unless deer are eradicated or severely reduced.
- The density of ticks is more sensitive to the availability of hosts for subadult ticks (small mammals and birds) than hosts for adult ticks.
- Woodland rodents carrying the bacteria that cause Lyme disease, especially white-footed mice and eastern chipmunks, are most likely to infect larval and nymph stages of black-legged ticks (Ixodes scapularis).
- People are most likely to contract Lyme disease from the bite of an infected nymph.
- Excluding deer can affect tick density. In areas smaller than 6 acres, the absence of deer may increase tick numbers. Exclusion from areas larger than 6 acres may decrease ticks numbers.
- Analysis of data from 4 states including Pennsylvania shows no relationship between the spatial distribution of Lyme disease and deer abundance.
- There is no clear relationship between deer density, tick abundance, and Lyme disease incidence.