Rabies
Guide to Rabies in PennsylvaniaRabies Virus - What You Need to Know
Cause
Rabies is caused by a virus that can affect the central nervous system of any mammal. The virus is usually transmitted in saliva via the bite of an infected animal.
Significance
Rabies is a great public health concern because it can be transmitted to humans by the bite of infected animals and is nearly 100% fatal without post exposure treatment. In the 1960s wildlife became the primary source of rabies exposure for domestic animals and humans. Cases of human rabies in the United States have declined with vaccination of domestic animals. With shrinking wildlife habitat and more opportunities to encounter wildlife, avoiding wild animals that are behaving abnormally is very important.
Species Affected
All mammals can potentially become infected with the rabies virus. In North America, the major wildlife reservoirs for this disease are raccoons, coyotes, skunks, bats, and foxes. Unvaccinated domestic or feral cats and dogs are also at risk of acquiring and transmitting rabies. For more information, including monthly Animal Rabies Reports, please visit the
Pennsylvania Department of Health's Rabies webpage.
Distribution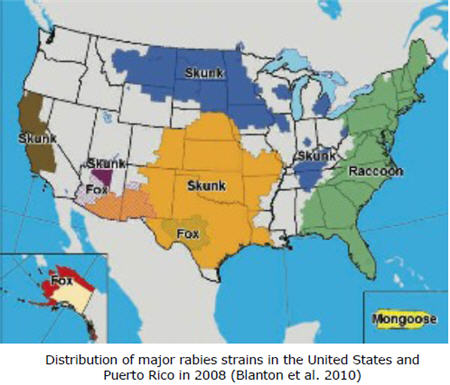
Rabies was probably introduced to North America from Europe in the 1700s. Rabies is currently found on every continent. The United Kingdom and Japan successfully eradicated rabies. Some other island nations are also free of the disease. There are multiple strains of the virus associated with particular wildlife species; the raccoon strain is most common in the Eastern United States. Skunk rabies is more common in the central United States and California, while fox rabies is found in Texas, Arizona, and Alaska. Raccoon rabies was first recognized in Pennsylvania in the 1980s and has since become established in the wild raccoon population. Since 1995 more than 350 animals have tested positive for rabies in the state each year; in 2010 there were 409 domestic and wild cases. Although raccoon rabies is very common in the region, this strain of the virus has only been reported in three cases of human infection. Most human cases in the United States and Canada are caused by bat rabies. Bats are a particular concern because their teeth are so small that people often do not realize that they have been bitten.
Transmission
Rabies is usually transmitted in saliva via the bite of an infected animal. Rabies may also be transmitted by non-bite exposures, which include infected saliva entering an open wound or the eyes or mouth. Rabies transmission has been reported in rare cases via inhalation of infected particles, and transplantation of infected tissue.
Clinical Signs
The incubation period of rabies is usually 1-3 months, but can vary greatly from species to species. This is the amount of time it takes for the virus to move from the site of exposure along the nerves to the brain where it produces great quantities of virus which subsequently spread first to the salivary glands and then other tissues. Non-specific neurologic signs usually follow the incubation period. Infected animals may exhibit abnormal behavior such as excitability, apparent lack of fear, or aggression. This is known as furious rabies. Furious rabies may progress to dumb rabies, or the animal may directly develop dumb rabies. Dumb rabies is characterized by loss of coordination and paralysis, which will eventually lead to coma and death within 1 to 10 days of onset of clinical signs. Sometimes infected animals will appear normal. Clinical signs can vary widely and resemble many other neurological conditions, so a diagnosis cannot be reached based on clinical signs alone. Generally speaking, abnormal behavior is the most common sign.
Diagnosis
Rabies diagnoses cannot be accurately determined in live animals, so rabies suspects must be euthanized and submitted for laboratory testing. The brain must be intact and should be refrigerated (not frozen) before testing. The brain tissue is tested using a fluorescent antibody test (FAT), which detects antibodies against the rabies virus.
Treatment
There is no generally accepted treatment for rabies, though 1-3 individuals are thought to have survived in recent years.
Management/Prevention
Prevention through vaccination has been very successful in domestic animals. People with greater risk of exposure such as veterinarians, wildlife biologists, wildlife rehabilitators, and animal handlers may receive pre-exposure vaccinations. If bitten by a possibly rabid animal, the wound should be washed thoroughly with soap and water and medical attention should be sought. If post-exposure treatment is administered before clinical signs appear, the development of rabies will be prevented nearly 100% of the time.
Oral Rabies Vaccine (ORV) programs have been implemented throughout the country to prevent further geographic spread of the virus. This program aims to vaccinate wildlife against rabies by distributing oral rabies vaccines within fishmeal bait. ORV programs have successfully eliminated fox rabies in several countries in Europe and in Texas. Pennsylvania began distributing ORV in 2001 in hopes of preventing further westward spread of the virus into Ohio.
Suggested Reading
Blanton, J. D., D. Palmer, and C. E. Rupprecht. 2010. Rabies surveillance in the United States during 2009. Journal of the American Veterinary Medical Association 237: 646-657.
Bureau of Epidemiology, Division of Infectious Disease Epidemiology. 2010. Pennsylvania annual animal rabies testing report 2010. Pennsylvania Department of Health, Harrisburg, Pennsylvania, USA.
Centers for Disease Control and Prevention (CDC). 2011. Rabies. http://www.cdc.gov/rabies/index.html.
Jackson, A. C. 2008. Rabies. Neurologic Clinics 26: 717-726.
Michigan Department of Natural Resources. Wildlife Disease. Rabies. http://www.michigan.gov/dnr/0,1607,7-153-10370_12150_12220-27259--,00.html.
Rupprecht, C. E., K. Stohr, and C. Meredith. 2001. Rabies. Pages 3-36 in E. S. Williams and I. K. Barker, editors. Infectious diseases of wild mammals. Iowa State University Press, Ames, Iowa, USA.
Slate, D., T. P. Algeo, K. M. Nelson, R. B. Chipman, D. Donovan, J. D. Blanton, M. Niezgoda, C. E. Rupprecht. 2009. Oral rabies vaccination in North America: opportunities, complexities, and challenges. PLoS Neglected Tropical Diseases 3: 1-9.
Wildlife Services. 2007. Cooperative Rabies Management Program National Report 2007. United States Department of Agriculture Animal and Plant Health Inspection Service.
Williams-Whitmer, L. M., and M. C. Brittingham. 1996. Rabies. Wildlife Damage Control 1. The Pennsylvania State University, University Park, Pennsylvania, USA.